Training Model
Our program uses a competency-based advancement model for graduate medical education training. The curriculum is deliberately structured to help residents develop progressive autonomy through the program’s educational philosophy of “learner,” “manager,” and “teacher / leader” phases. Each phase is focused on a different set of responsibilities and level of competencies.
Learner: In the learner phase of training, the trainee works on basic milestones in patient care. They are supervised directly by upper-level trainees or attending physicians. They are challenged to advance their skills in history, physical diagnosis, diagnostic reasoning, management, teamwork, and systems-based practice. Supervisors are trained in the principles of “supervised autonomy” so that learners are not directed, but rather coached, to grow in these milestones.
Manager: Once a learner reaches competency in all learner milestones, they advance to the manger phase of training. In this phase, each trainee works to establish independence in patient care knowledge and skills. In most rotations, managers do not supervise learners, nor are they supervised by upper-level residents. They work collaboratively with attending physicians to establish competence in management of common medical conditions in both inpatient and ambulatory settings in both medicine and pediatrics. Most residents consider this to be the most challenging but also most rewarding phase of training as they truly grow into clinical independence.
Teacher / Leader: Once a resident is considered independent in managing most common medical conditions, they advance to the teacher / leader phase of training. In this phase, they continue to gain the necessary experience over time in managing many medical conditions, but they also work on refining teaching and leadership skills. Their milestones during this phase are worded as phrases such as “can teach others", ”leads a healthcare team", “coordinates care", and “role models for others". It is at this phase of training that our residents lead teams on wards and ICUs, specialize in consultative care, and serve in advanced roles in the ambulatory care setting.
Training Curriculum
The 48-month curriculum of the VCU Med-Peds Residency Program is designed to meet the requirements established by the American Boards of Internal Medicine and Pediatrics, leading to board eligibility in both disciplines. All interns start on internal medicine rotations together. Residents then switch between departments every three to six blocks. A sample rotation schedule is shown below, where each block represents 4 weeks of time.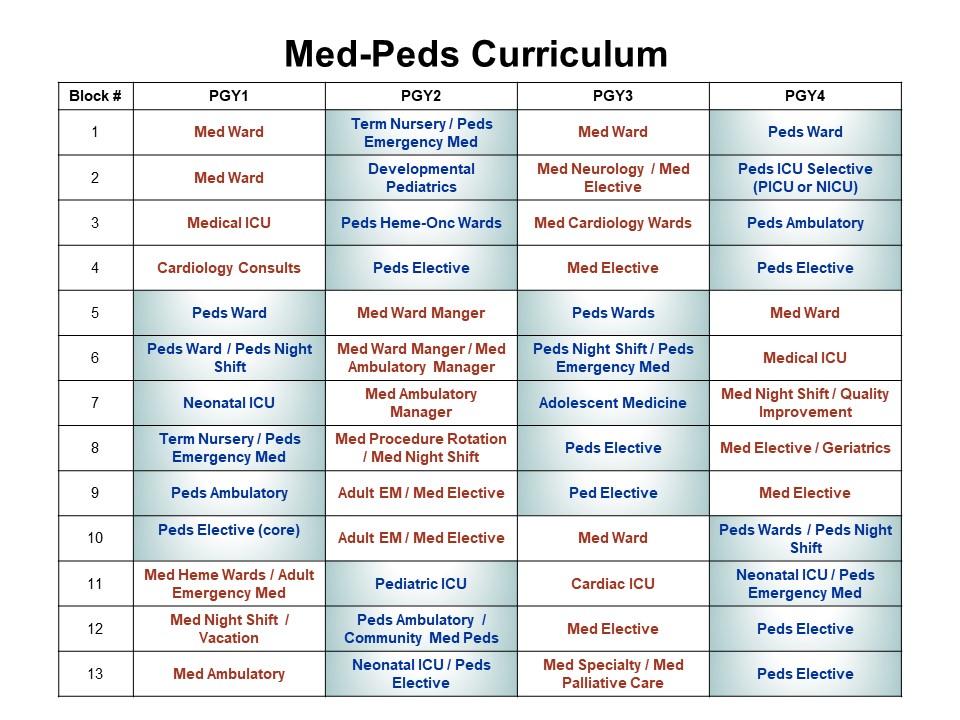
Pediatric rotations are shaded blue; internal medicine rotations are shown in red. Medicine ambulatory manager rotations include outpatient geriatrics, community-based med-peds practice, and underserved medicine. Medicine neurology in the PGY3 year is also an ambulatory experience. We offer extensive elective offerings in both medicine and pediatrics, including all typical subspecialty experiences as well as many unique opportunities.
Tandem Block Schedule
The curriculum is modeled on a unique tandem block schedule that alternates every two weeks between inpatient rotations (wards, intensive care units) and other learning experiences (ambulatory, elective, consult services, research, or shift work). The tandem block schedule was designed by our residents with the following goals in mind:
- Separate inpatient and ambulatory responsibilities with dedicated curricula
- Preserve inpatient teams for teamwork and evaluation purposes
- Minimize hand-offs during inpatient rotations
- Ensure appropriate emphasis on ambulatory, elective, and other non-inpatient experiences
- Provide elective time so that residents may pursue areas of interest by tailoring rotations to individual academic and career goals
- Enhance continuity in continuity clinic
- Reduce burn-out and fatigue
- Maximize work-life balance
In the tandem block schedule, each four-week block (based on the curriculum diagram above) is further divided into two-week blocks (A/B), represented by each column in the example below. During any 8-week period, a resident completes two full rotations. This example shows the first sixteen weeks of the year, after which an intern would rotate to pediatrics.
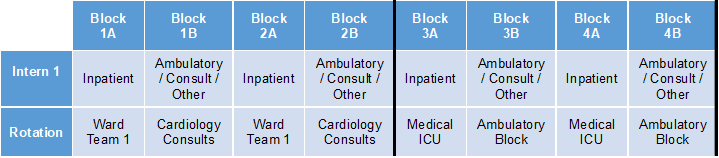
In most cases, the team members (i.e. senior resident and co-intern) are the same for blocks 1A and 2A. Team members would be different for blocks 3A and 4A in the ICU, but the goal of preserving the team structure still holds.
Residents typically have two half-day sessions of continuity clinic during each week of non-inpatient rotations. They do not have continuity during inpatient rotations.

